Equine dentistry is an area of the veterinary field that is performed both by veterinarians and qualified equine dental technicians. Dental technicians can perform routine checks and rasp teeth but other procedures, such as extractions, must be carried out by a veterinarian. There are pros and cons for each role, which are outside the scope of this article.
The investigation of every dental case should start with a detailed oral examination. This often begins with dental radiographs, instead of starting with the very beginning: looking in the horse's mouth (Limone, 2022). In omitting the visual examination, the vast amount of information that can be gained from an oral examination is lost. This article focuses on the importance of the visual oral examination. Special emphasis will be placed on examining the dental structures visible on the occlusal surface of the cheek teeth and common pathology affecting these dental structures.
When performing an oral examination, the mouth should be flushed out and the horse should be sedated. Owners are often reluctant to allow sedation at first, but if the horse is not sedated, a full, professional oral examination cannot be effectively peformed. In the author's opinion, horses tolerate floating their teeth better than they tolerate a mirror in their mouths – and movement of the tongue or chewing is counterproductive when attempting to look in the mouth with a mirror. In the literature and the author's communications with veterinarians who routinely perform oral examinations, this is not negotiable (Menzies, 2013; Limone, 2022). Subtle, though vitally important pathology such as pulp exposure, might be missed if the horse is not sedated. This gives veterinarians a distinct advantage over equine dental technicians who cannot sedate horses.
If a single piece of equipment is a game changer in equine dentistry, it is a dental endoscope or dental camera. A camera allows for a detailed examination of all the teeth and soft tissue structures while recording the data. Images are magnified and viewed on a screen, compared to the reflection in a dental mirror. Using the images, the anatomy and pathology can be explained to the owner. Many dental endoscopes also give the option to rotate the image to an anatomically correct position, allowing the vet to work in the mouth with instruments while looking on the screen, similar to arthroscopy (Easley, 2022).
However, one does not need a scope – a sufficient oral examination can be performed without a significant additional investment. The minimum equipment required is a speculum, dental mirror, headlamp, bucket with water and disinfectant, and a dental pick/explorer (Menzies, 2013; Limone, 2022). A headstand or dental halter will make the procedure much more comfortable for both the veterinarian and the horse.
A dental mirror is a must (Menzies, 2013; Limone, 2022). Without a mirror, the occlusal and peripheral surfaces of the teeth cannot be adequately examined. Various dedicated equine dental mirrors are available, with or without magnification. It is quite possible to make a dental mirror for little investment: use a human dental mirror and handle, which is cheap and freely available, and add a 30–40 cm extension (aluminium tubing works well) for a longer handle (Figure 1). The small mirror heads are cheap, easily replaceable and fit into small spaces, allowing for detailed examination of areas often inaccessible with larger equine dental mirrors. The one disadvantage is that the occlusal surface cannot be viewed as a whole. In terms of lighting, a bright camping headlamp works very well. The more dedicated (and expensive) headlamps allow for better illumination exactly where the veterinarian is looking, as the LED is on a bendable arm and the light source is situated lower down between the eyes (Limone, 2022).

Before placement of the speculum, the external head, mandible and temporomandibular joints should be palpated and the nostrils checked for nasal discharge. The incisors should be examined, as the occlusal surfaces will be obscured by the bite plates (Limone, 2022). Clinical signs of a diseased incisor include gingivitis, gingival recession, mobility or an exposed pulp (following the same principles for exposed pulp in cheek teeth). In advanced cases, bulging of the gingiva and draining tracts may be evident, as seen in equine odontoclastic tooth resorption and hypercementosis (Dixon et al, 2022a).
Once the speculum is in place, the oral cavity should be flushed out well. The cavity should then be visually examined to get an impression of the anatomy, the occlusal surface angles, focal overgrowths or trauma to the soft tissue structures. The occlusal surfaces should also be palpated as this provides excellent information regarding the three-dimensional topography. There should be six cheek teeth in all four arcades in the normal horse over the age of 3.5–4 years; wolf teeth (premolar one) may or may not be present in the upper quadrants (Limone, 2022).
The next step is a detailed examination with a dental mirror or dental endoscope. The interdental spaces and gingiva should be examined for the presence of diastemata, periodontal pocketing and draining tracts (Dixon et al, 2022a). Four different mineralised dental structures are visible on each occlusal surface: cementum, enamel, primary dentine and secondary dentine (Dixon et al, 2022b). Pathology of each of the various structures has different implications. In horses, the periphery of the occlusal surface and clinical crown are covered by cementum, as the teeth are continuously erupting – this is in contrast to brachydont teeth, where only the clinical crown is covered by enamel. The cementum, which is the softest mineralised part of the tooth, has a relatively high collagen content and protects the brittle peripheral enamel (Figure 2). The peripheral enamel lines the primary dentine (Dixon et al, 2022b). In addition, the maxillary cheek teeth have two irregularly-shaped complete enamel rings (infundibular enamel) filled with cementum, called the infundibula (singular: infundibulum) (Figure 2). The infundibular enamel provides extra enamel ridges, increasing the grinding surface of the tooth (Figure 3) (Suske et al, 2016a).
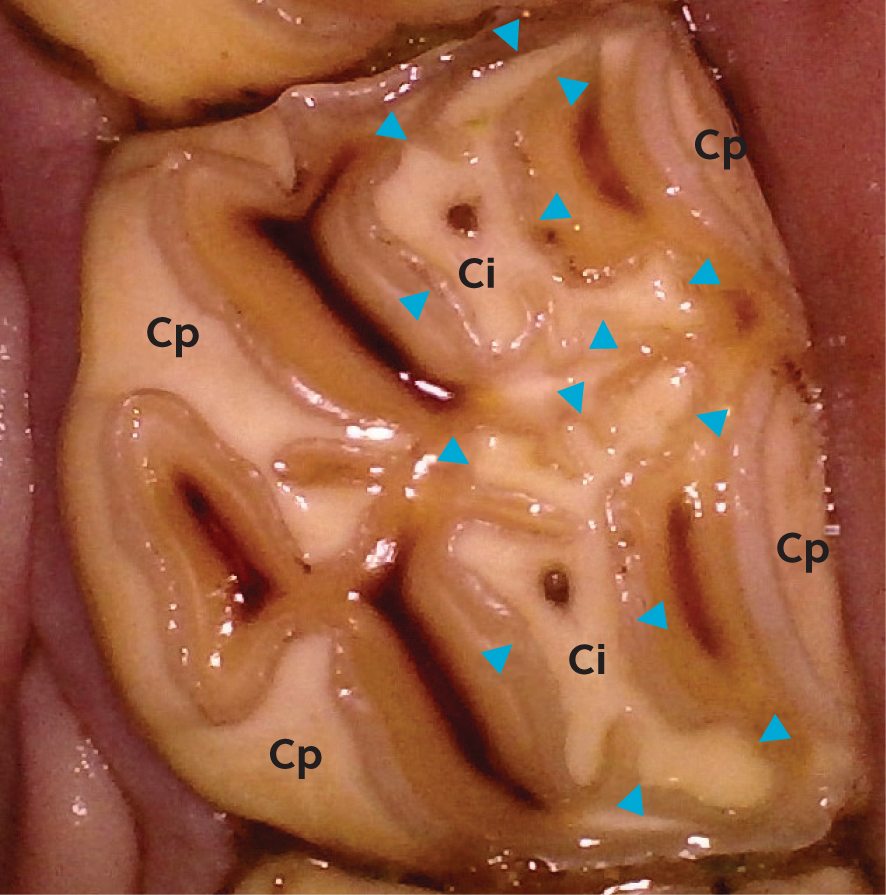
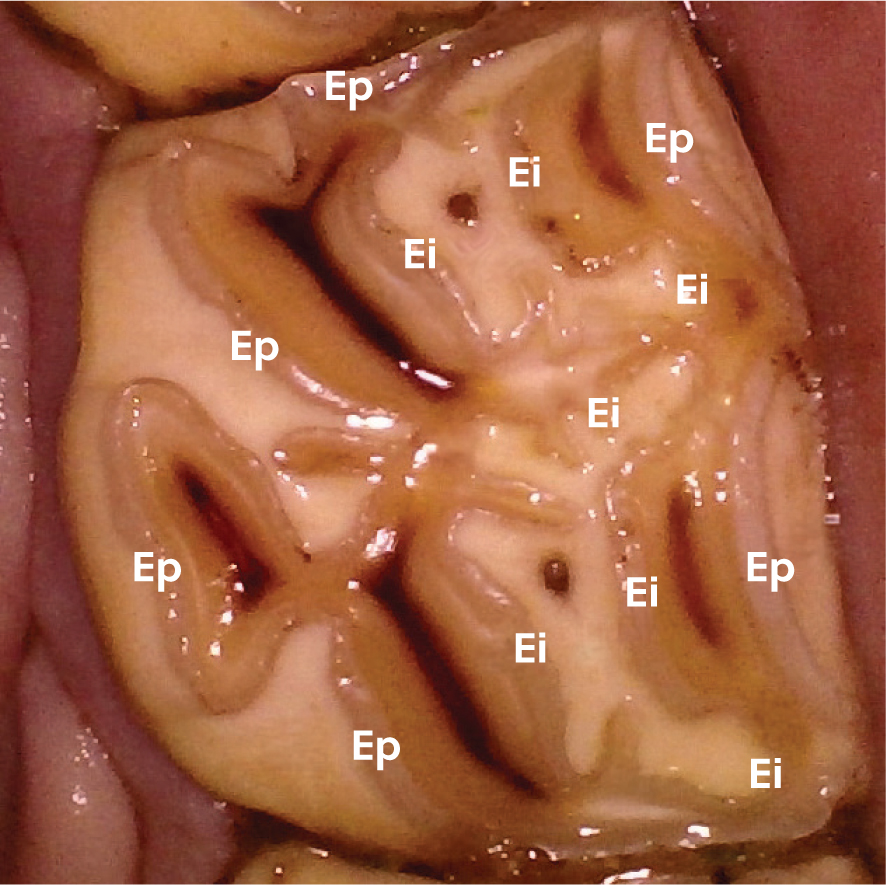
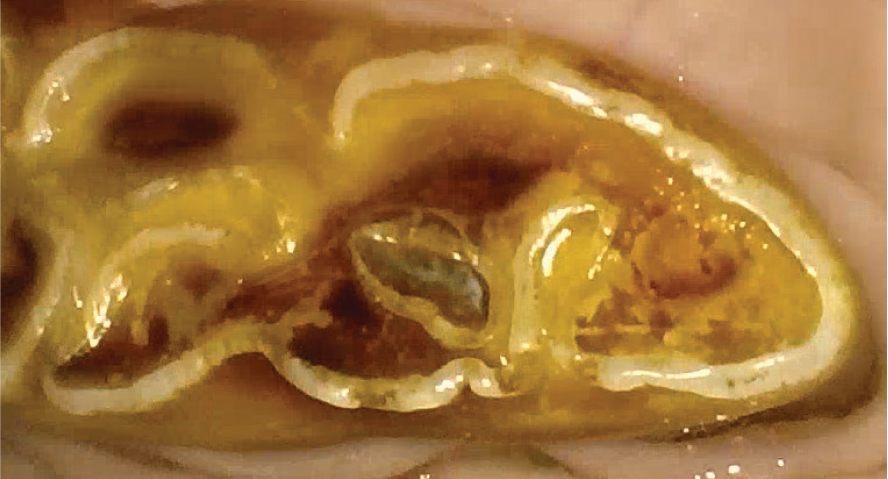
Primary dentine makes up the bulk of the tooth. On the occlusal surface, primary and secondary dentine are distinguishable (Figure 4). The secondary dentine can be seen as dark brown slits, marking the pulp horns, surrounded by light brown primary dentine (Dixon et al, 2022b). Each cheek tooth has 5–7 pulp horns (Du Toit et al, 2008) (Figure 5).

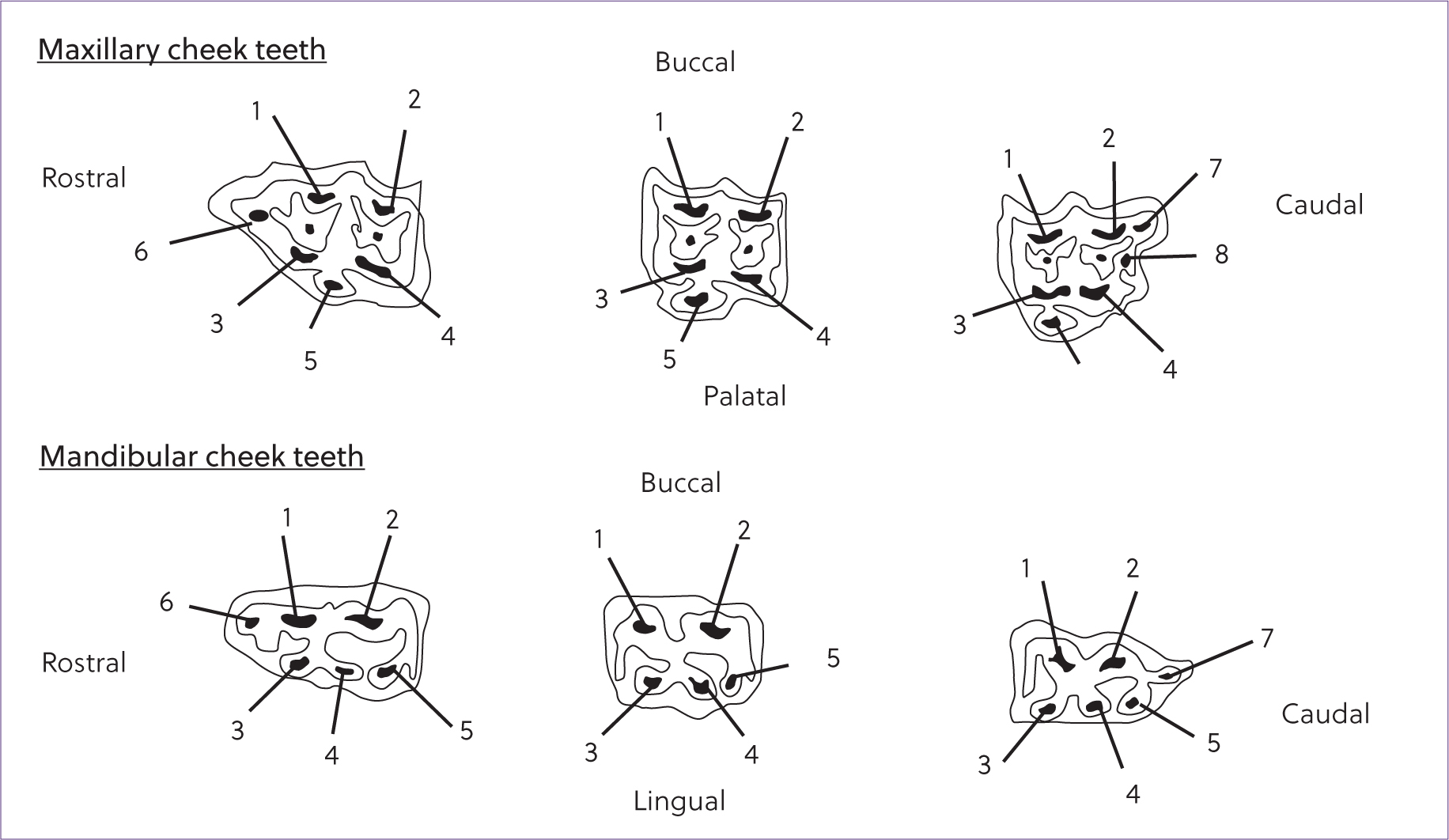
It is vital to know where the pulp horns are and what they should look like. For the maxillary arcades, Triadan 07–10 are the same, with five pulp horns each. Maxillary Triadan 06s have an additional pulp horn mesially (which could easily be damaged with over-aggressive bit seating or hook reduction) and the 11s have an additional pulp horn distally (Du Toit et al, 2008). Likewise, the mandibular Triadan 07–10s all have five pulp horns, 6 has an additional pulp horn mesially and 11 has two additional pulp horns distally (Du Toit et al, 2008) (these can be compromised during over-aggressive caudal mandibular ramp reduction).
Primary dentine lines the inside of the pulp cavity for the tooth's length; on the occlusal surface, the pulp is sealed with secondary dentine. As the tooth erupts (and keeps erupting in these hypsodont teeth) and wears down, the secondary dentine is deposited towards the occlusal surface of the pulp cavity to prevent pulpar exposure (Dixon et al, 2022b). The thickness of the subocclusal secondary dentine varies greatly and can be as little as 3 mm (White and Dixon, 2010); this should be taken into account when reducing overgrown teeth. The secondary dentine takes up pigment from food, giving it a dark brown appearance (or occasionally black, when grazing on certain pastures) (Dixon et al, 2022b).
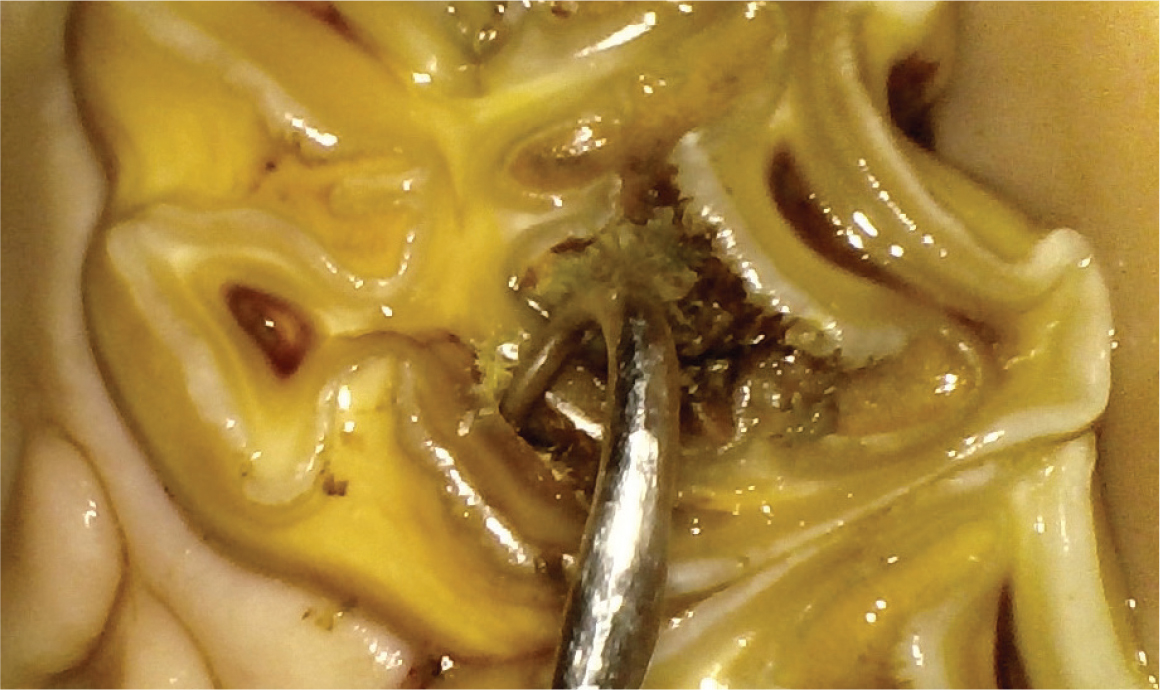
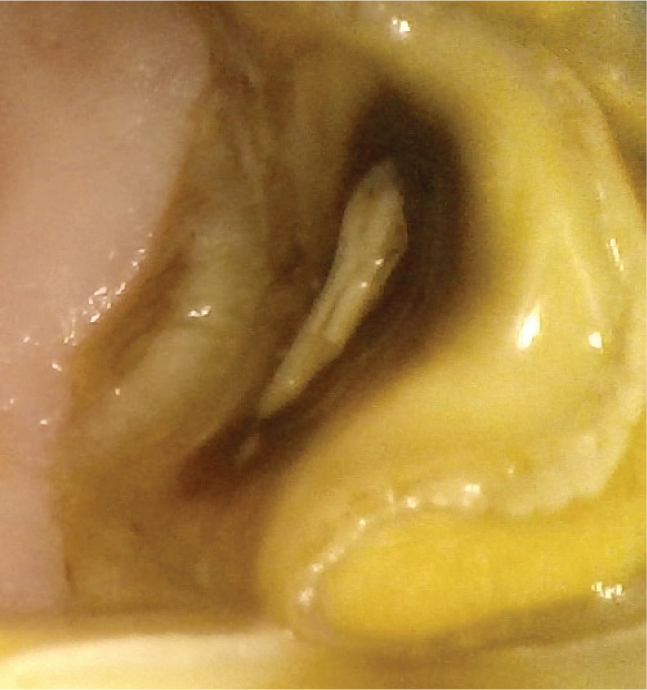
The dark brown secondary dentine, with a slightly brighter centre, should be solid and hard (Dixon et al, 2022b). If a defect is present in the secondary dentine, the tip of a dental pick will sink into it with probing (Figure 6) (Dixon et al, 2022a). When abnormal, with an exposed pulp, food often adheres to it, or a white edge is visible (Figure 7). These teeth should be probed with the dental pick to confirm the defect in the secondary dentine and radiographed. A common pathology visible on the occlusal surface of cheek teeth is infundibular caries of the maxillary teeth and fractures. Peripheral caries can also be appreciated occlusally, although it is better seen on the periphery of the teeth, which should also be examined (Dixon et al, 2022b). This is often associated with diastemata and periodontal disease (Borkent et al, 2017).
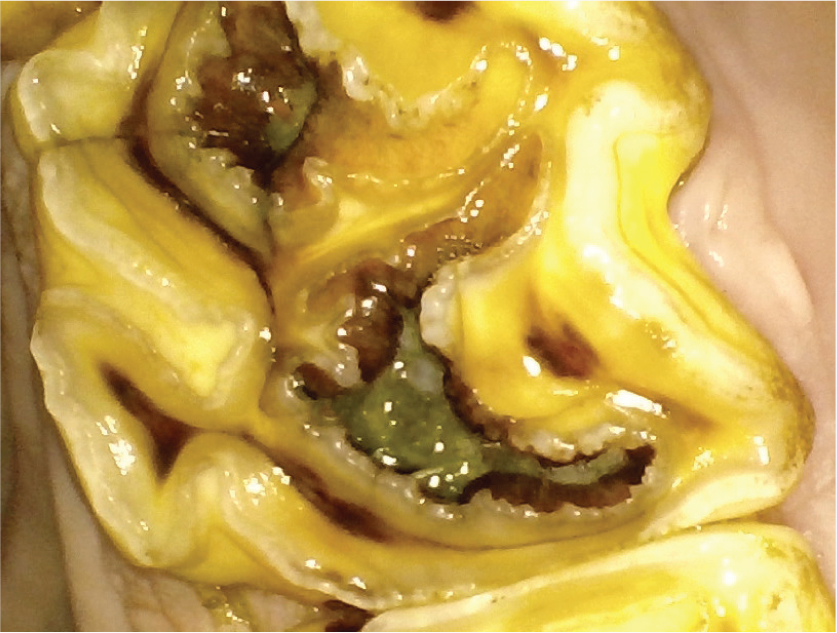
The infundibula are commonly affected by cemental hypoplasia and infundibular caries (Figure 8). Many cheek teeth infundibula are incompletely filled with cementum (Suske et al, 2016a; 2016b; Horbal et al, 2017). In addition to this weakness in the cementum, food material will become impacted in these voids, acting as a port of entry for acid-producing bacteria, leading to demineralisation of the dental structures (Pearce and Horbal, 2022). The softest of the structures, cementum, is affected first (grade 1); as the disease progresses, it extends into the enamel (grade 2) and dentine (grade 3). Grade 4 occurs when there is a coalescence of the mesial and distal infundibula, and grade 5 is when the tooth has fractured because of advanced caries (Pearce and Horbal, 2022). Infundibular caries can be treated, and these teeth prevented from fracturing, by performing infundibular restorations on teeth with grade 3 infundibular caries that is at least 10 mm deep. A tooth with grade 2 infundibular caries with a depth of at least 10 mm, contralateral to a tooth with grade 5 infundibular caries should also be considered for infundibular restoration. Teeth with periapical infection or that are associated with a nasal discharge (in the past or present) should not be restored (Pearce and Brooks, 2022). Similar to infundibular caries, peripheral caries is often seen affecting the cementum, enamel and, to a lesser extent, the dentine (Dixon et al, 2022a).
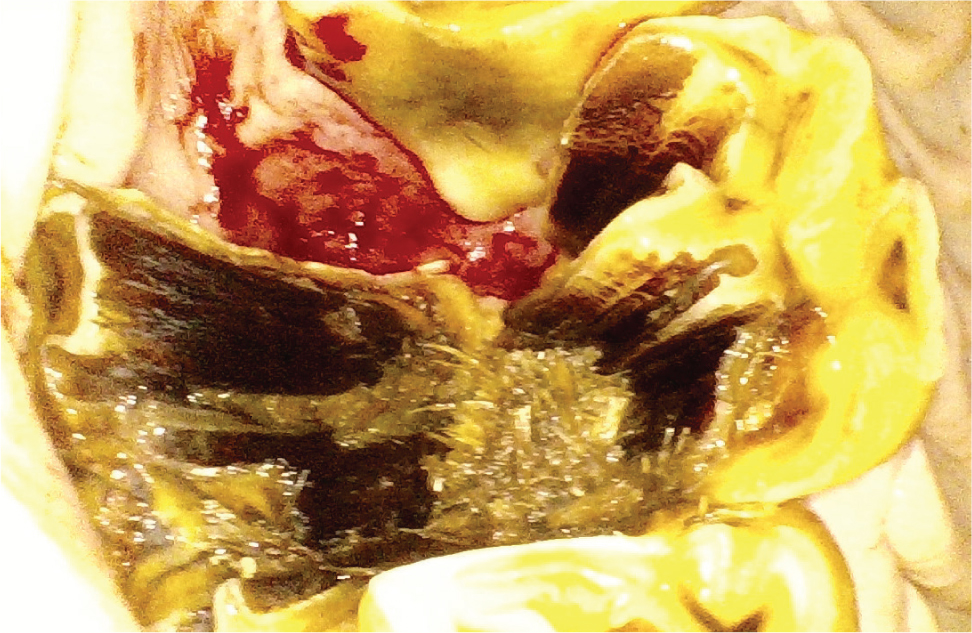
When a cheek tooth fractures as a result of infundibular caries, it is a clear-cut decision that it requires extraction (Figure 9). With other cheek teeth crown fractures, decision making will revolve around whether the pulp is exposed or not (Vlaminck and Pollaris, 2022). If a fracture involves the secondary dentine, it should be probed. If the secondary dentine has no defect, which is often seen with fractures that do not extend below the gingival margin, obtaining radiographs is not essential. However, if a secondary dentine defect is present, the pulp is exposed and the tooth should be radiographed. If apical changes are present, the tooth should be extracted (Vlaminck and Pollaris, 2022).
Sometimes, although the pulp may have been exposed, the body is able to form a tertiary dentine bridge to seal off the pulp and prevent apical infection (Dixon et al, 2022b). In these cases, radiographic changes might not be present. The best treatment protocols for these cases are controversial, with the options being to perform a root canal restoration, extraction or to simply monitor the tooth (Vlaminck and Pollaris, 2022). Ultimately, treatment will depend on the clinician's experience and preference, and the client's expectation and budget.
Fissures or cracks on the occlusal surface are common in cheek teeth, with a reported prevalence of up to 72% (Pollaris et al, 2018); the different configurations have been described well. These are incidental findings, although fissures could form a weak spot and predispose to fracture (Ramzan and Palmer, 2010; Vlaminck and Pollaris, 2022).
Careful evaluation of the occlusal surface could also give a clear indication of a horse not chewing properly, as a result of pain. This is sometimes seen as a different staining pattern on the teeth (Figure 10). More commonly, a difference in the occlusal surface angle (left vs right) might be visible. Horses with dental pain adopt a more vertical chewing action, instead of lateral movement, or may choose to only chew on one side of the mouth. This creates uneven wear of the left vs right occlusal surfaces, which in neglected cases, results in a sheer mouth (Figure 11) (Dixon et al, 2022a). In these cases, the underlying problem should be addressed, instead of only trying to reduce the overgrowths.

Conclusions
A detailed examination of the occlusal surfaces of the equine cheek teeth can yield substantial information, which will be very useful in decision making regarding dental procedures.


