The cardiovascular system of the equine neonate undergoes several changes at birth and different conditions can impact the heart's function, sometimes requiring prompt intervention. With very different features than in adulthood, it is important to differentiate normal from abnormal clinical findings in the equine neonate to adopt the most appropriate clinical approach. This article reviews the key aspects in equine neonatal cardiology for the equine practitioner.
From fetus to foal
During intrauterine life, fetal circulation allows for oxygen and nutrient transport from the placenta through the umbilical vein (Figure 1) (Tan and Lewandowski, 2020). Oxygenated and nutrient-rich blood circulates to the liver via the ductus venosus, which connects the umbilical vein to the caudal vena cava, before entering the right atrium (Tan and Lewandowski, 2020). Blood that enters the right atrium is then directed through the foramen ovale to the left atrium, forming a right-to-left shunt proximal to the ventricles and bypassing the lungs (MacDonald et al, 1988; Tan and Lewandowski, 2020). In the left atrium, blood mixes with less oxygenated blood arriving from the pulmonary veins from the non-functional fetal lungs (Hyttel, 2010). Blood enters the left ventricle from the left atrium and is pumped throughout the systemic arterial network with preferential supply to the brain and heart (Hyttel, 2010).
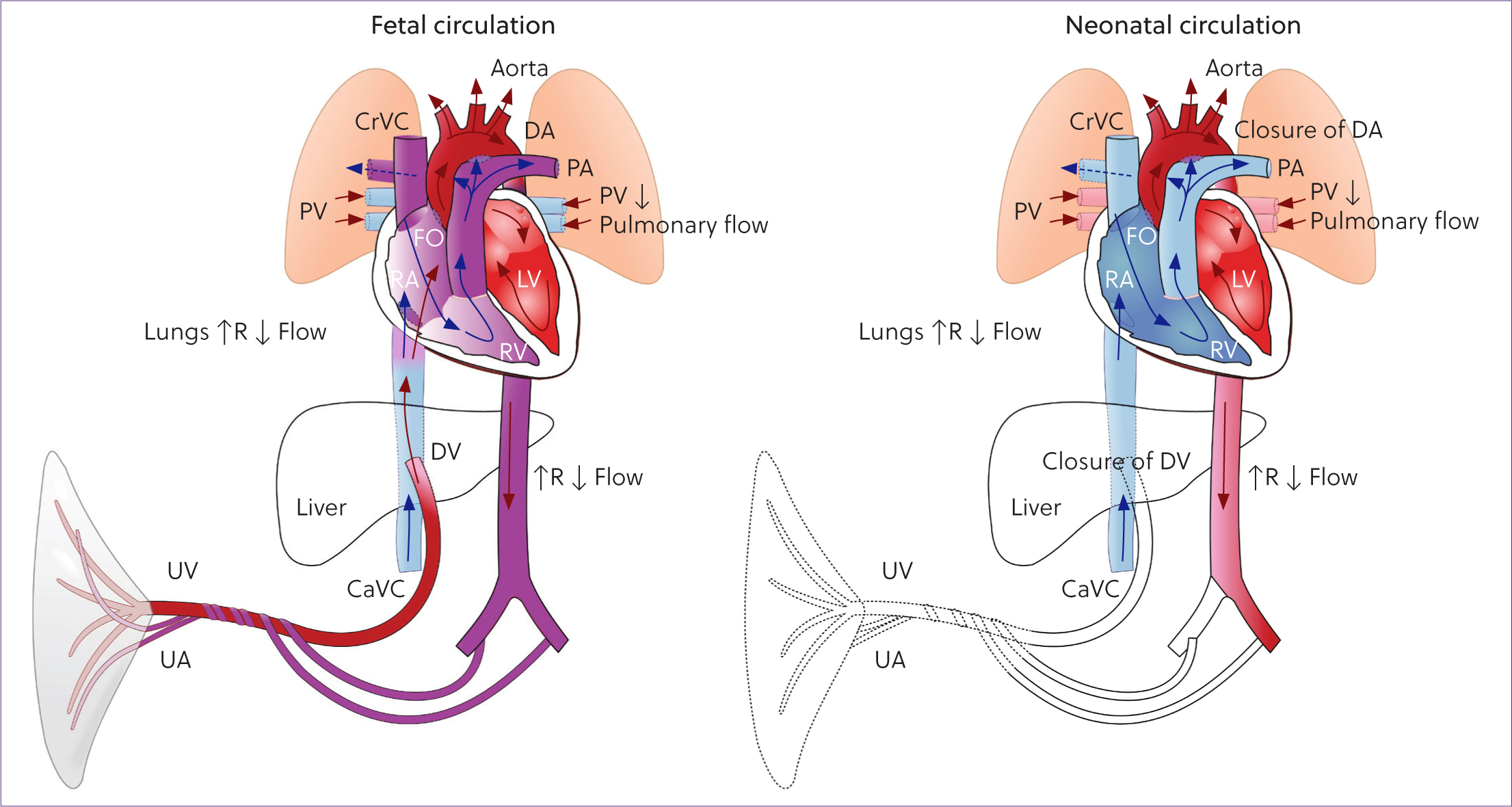
Some of the blood arriving from the caudal vena cava into the right atrium does not pass through the foramen ovale, instead entering the right ventricle and mixing with deoxygenated blood which returns from the head of the fetus via the cranial vena cava, and the myocardium via the coronary veins (Scott, 2020). The blood from the right ventricle is pumped into the pulmonary trunk and, because of the high vascular resistance within the non-inflated fetal lungs, most of this blood enters the aorta via the ductus arteriosus, a right-to-left shunt distal to the ventricles (Hyttel, 2010). The partially oxygenated blood in the aorta returns to the placenta via the paired umbilical arteries after supplying the thoracic and abdominal organs (Scansen, 2019).
Important circulatory changes occur at birth. First, the contraction of the umbilical arteries and veins forces blood towards the foal's circulation. Placental blood can contribute up to 30% of the neonate's total blood volume, so the umbilical cord should not be clamped or cut too quickly after birth (Scott, 2020). Second, hypoxaemia and hypercapnia induce the first gasping breaths that inflate the lungs and expel the fetal fluids from the lungs (Hyttel, 2010; Scott, 2020). The decrease in pulmonary vascular resistance causes blood from the pulmonary trunk to flow to the pulmonary arteries, instead of through the ductus arteriosus, and become oxygenated in the lungs (Tan and Lewandowski, 2020). As a consequence of the cardiorespiratory and hormonal changes at birth, a thin layer of tissue initially closes the foramen ovale and ductus arteriosus, eliminating the right-to-left shunts, and separating the pulmonary and systemic circulations in the newborn foal (Loberg, 2010; Marr, 2015). These shunts will permanently close over a few weeks, if the foal is healthy (Loberg, 2010; Scansen, 2019). However, these shunts can reopen when a foal experiences severe pathology (Loberg, 2010).
Heart rate and rhythm
The healthy equine neonate has a heart rate of around 70–110 bpm during its first week of life, which may vary considerably with activity or excitement (Table 1) (Magdesian, 2014; Marr, 2015). However, in states of disease (eg hypovolaemia, sepsis, anaemia) when a rise in pulse rate is expected, foals may fail to mount this protective physiological response. Some hypovolaemic foals will maintain a normal heart rate, resulting in a reduced cardiac output and inadequate oxygen delivery to the tissues, increasing the risk of morbidity and mortality (Corley, 2003; Bernard and Barr, 2012).
| Age | Heart rate (bpm) |
|---|---|
| Fetus | 62–140 |
| After delivery <10 minutes | 40–80 |
| If active (eg attempting to stand) | 130–150 |
| <12 hours | 100–200 |
| 24 hours | 80–100 |
| First week of life | 70–110 |
| Few weeks to months | 60–80 |
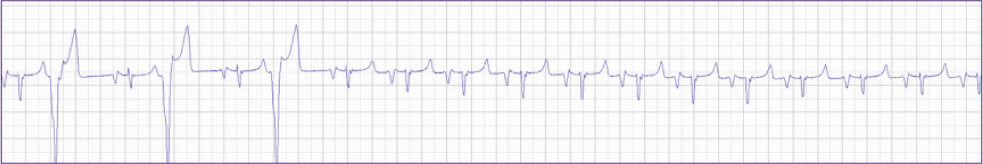
During the first 15 minutes postpartum, healthy foals can transiently have a wandering pacemaker, supraventricular premature depolarisations, supraventricular tachycardia, atrial fibrillation, ventricular premature depolarisations, ventricular tachycardia and second-degree atrioventricular block, so monitoring the rhythm is warranted (Madgesian, 2014; Cruz et al, 2015; Marr, 2015). Prompt intervention is required if a compromised neonate has a heart rate lower than 50 bpm, because sinus bradycardia can progress to electromechanical dissociation and asystole can occur (Marr, 2015). Emergency therapy consists of cardiac compressions, administration of adrenaline (0.005–0.01 mg/kg intravenously or 0.05–0.1 mg/kg intratracheally) and atropine (0.005–0.01 mg/kg intravenously) and, if the material is available, transcutaneous pacing (Javsicas and Giguère, 2008; Jokisalo and Corley, 2014; Marr, 2015).
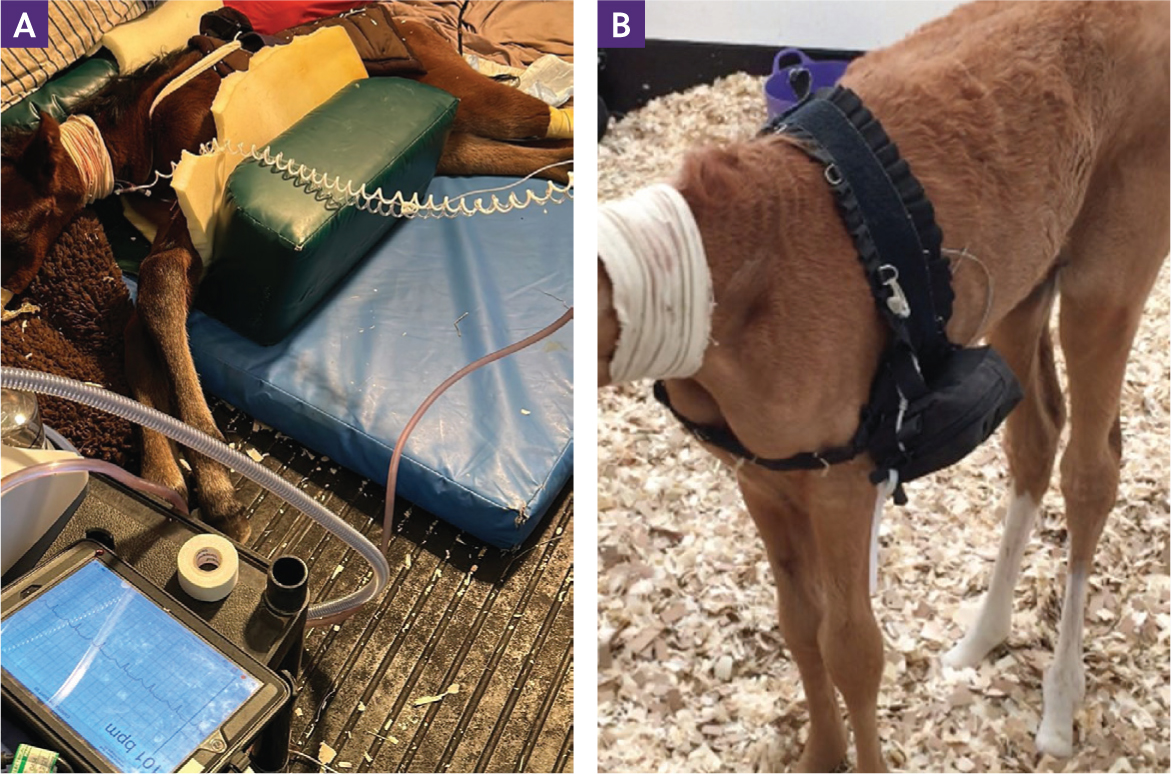
Most arrhythmias in foals are secondary to systemic disease (Figures 2 and 3) (Bernard and Barr, 2012). Bradycardia in foals is mostly associated with tissue hypoxia (eg dystocia or severe anaemia), hypothermia, hypoglycaemia (eg sepsis) or hyperkalaemia (eg uroperitoneum) (Corley, 2003; Marr, 2015; Conze et al, 2022) (Table 2).
| Auscultatory finding | Timing | Point of maximal intensity (valve area)a | |
|---|---|---|---|
| Normal heart sounds | |||
| First heart sound (S1) | Onset S |
|
Left apex (mitral valve) |
| Second heart sound (S2) | End S | Left base (aortic valve) | |
| Third heart sound (S3) | Early D | Left apex (mitral valve) | |
| Fourth (atrial) sound (S4) | Late D | Ventricular inlet or base (left) | |
| Physiological murmurs* | |||
| Systolic ejection murmur | S |
|
Left base (aortic/pulmonary valves) |
| Patent ductus arteriosus | S + D |
|
Dorsal left base over pulmonary artery |
| Pathological murmurs | |||
| Ventricular septal defect † | S |
|
Right sternal border/left cardiac base |
(adapted from Schwarzwald, 2018)
Apex refers to the ventral part of the heart, at the point of palpable cardiac impulse (apex beat); base refers to the craniodorsal part of the heart over the aortic and pulmonic valves where S2 is most intense (Figure 1) (Schwarzwald, 2018).
Murmurs caused by defects in the right ventricular inlet septum (paramembranous ventricular septal defect, common) are heard best above the right sternal border; murmurs from defects in the right ventricle outlet septum (subpulmonic ventricular septal defect, rare) may be loudest over the pulmonic valve; increased flow across the pulmonic valve can cause left-basilar systolic murmurs of relative pulmonic stenosis in the absence of pulmonic valve pathology; flow across very large non-restrictive defects can be relatively soft (Schwarzwald, 2018).
Treatment for tachyarrhythmias in foals is similar to that described for adults. Treatment recommendations for adult horses can be found in detail elsewhere (Redpath and Bowen, 2019; van Loon, 2019). However, with the advantage of their smaller size, techniques such as transcutaneous electrocardioversion are applicable in foals (Marr, 2015; Potter et al, 2017).
Heart murmurs
Because of the foal's thin chest, heart sounds and flow murmurs are louder than in the adult horse (Figure 4) (Bernard and Barr, 2012). There are three types of physiological flow murmurs audible in healthy foals at birth: flow through the great vessels, the foramen ovale and the ductus arteriosus.
Crescendo-decrescendo systolic soft blowing ejection murmurs are created by the turbulent ejection of blood from the heart in the great vessels or through the foramen ovale and are commonly heard in healthy foals until 2 weeks of age. Intensity can be as high as a grade III or IV, and localisation is over the heart base on both sides of the chest. The tone can sound unusual if the foal is in recumbency or haemodynamically compromised, which makes differentiation from pathological murmurs challenging (Bernard and Barr, 2012).
Continuous harsh machinery murmurs cranial and high over the left heart base are created by flow through the ductus arteriosus. Because this duct closes over the first days of life, this murmur may be pathological if heard after 4 days of age, although there is discrepancy in the literature around the closure of the ductus arteriosus (Marr, 2015; De Lange et al, 2022). Cardiac disease should be suspected in foals with persistent or loud, widely radiating murmurs with a precordial trill, and other clinical signs such as weakness, failure to grow and gain weight, dependent oedema, tachycardia, jugular distension and pulsation, pleural effusion, ascites, cyanosis, dyspnoea, bounding arterial pulse, syncope and collapse (Magdesian, 2014; Marr, 2015).
Blood pressure and pulse pressure
Jugular pulsation represents pressure changes in the thorax and right atrium and is visualised in healthy neonates from the thoracic inlet to the level of the shoulder. However, jugular veins should not be distended, and pulsation should not be seen above the shoulder (Reef, 1985). Strong arterial pulses are easily palpable over the metatarsal and axillary arteries in healthy foals. What is actually palpable is the pulse pressure, which is the difference between systolic and diastolic pressure, and is independent of their absolute values or the mean pressure (Bernard and Barr, 2012).
In foals, the pulse pressure palpable over the metatarsal artery is often reduced in states of hypotension, and palpation of faint pulses suggests the need for fluid therapy and cardiovascular support (Corley, 2003). However, the palpable pulse pressure may occasionally feel normal in hypotensive foals and may be misleading; for instance, if the diastolic pressure is low but the stroke volume remains reasonable. To overcome this limitation, measurement of blood pressure is recommended, especially in critically ill foals. Non-invasive blood pressure measurements are more accurate in foals than adults because of the thinner layer of soft tissue surrounding the peripheral arteries (Giguère et al, 2005). Non-invasive blood pressure measurements with automated oscillometric monitors at the level of the coccygeal artery have good accuracy; however, accuracy will decrease in severely hypotensive foals or when the tail cuff size is too large or too small (Giguère et al, 2005; Nógrádi and Magdesian, 2018). In critically ill foals, the general goal is to maintain mean pressures above 60–65 mmHg – this is also used as a threshold for intervention (Giguère et al, 2005; Nógrádi and Magdesian, 2018). Irrespective of the mean pressure, if hypovolaemia is refractory to fluid therapy, pressor therapy may be indicated even if pressures are above 60 mmHg.
Echocardiography
Echocardiography is routinely available in neonatal intensive care units, and studies have published echocardiographic measurements in foals by age and body weight (Stewart et al, 1984; Collins et al, 2010). In addition to the classic views performed in adults, a subcostal view is described and allows for better alignment with aortic outflow in foals (Freccero et al, 2018). Echocardiography is a non-invasive tool to evaluate congenital cardiac defects, acquired heart murmurs, pericardial, myocardial and endocardial disease (Reef, 1985).
Sedation in foals
Foals are particularly sensitive to sedatives, and sedation may precipitate events that will lead to cardiac arrest, especially in critically ill foals (Bernard and Barr, 2012). Some features related to their cardiovascular physiology are worth considering when sedating foals (Loberg, 2010). First, the neonatal heart is less capable of increasing myocardial contractility and stroke volume, so the foal's cardiac output relies more on heart rate. Second, as a result of the immaturity of the autonomous system and cardiac reflexes, foals have a lower capacity to compensate for haemodynamic changes while under sedation or anaesthesia (Fischer and Clark-Price, 2015). Third, the foal's immature renal, hepatic and neurological systems mean that the pharmacological effects of anaesthetic drugs can be exacerbated (Fischer and Clark-Price, 2015).
In neonates, profound sedation and restraint with benzodiazepines can be achieved and is preferred over alpha-2 agonists (Table 3). The latter will cause more cardiovascular depression, with a decrease in heart rate, mean arterial pressure and cardiac index, decreased gastrointestinal motility and perfusion, increased urine production and sodium and potassium loss (Loberg, 2010; Fischer and Clark-Price, 2015; Kerr et al, 2021). These effects worsen in cases of dehydration, sepsis or hypoxic ischaemic encephalopathy (Fischer and Clark-Price, 2015). Butorphanol can be used alone or in combination with benzodiazepines for procedures such as catheter placements or bandaging, or as premedication for anaesthesia (Figure 5) (Loberg, 2010; Fischer and Clark-Price, 2015). Acepromazine is commonly used as a mild sedative in adults, but should not be used in foals as it causes long-lasting hypotension, anaemia and decreased platelet aggregation (Fischer and Clark-Price, 2015).
| Foals 0–2 weeks old | Foals 2–4 weeks old | Foals older than a month |
|---|---|---|
| Butorphanol 0.1 mg/kg and diazepam 0.1-0.2 mg/kg intravenously | Xylazine 0.5 mg/kg and butorphanol 0.1 mg/kg intravenously If needed in healthy foals, use xylazine 0.5 mg/kg intravenously | Xylazine 1 mg/kg and butorphanol 0.05 mg/kg intravenously |
| Reversion of sedation | Flumazenil 0.5 mg intravenously | |
Acquired disease
Infection
Neonates and young foals are particularly susceptible to sepsis and multiple site infections, including in the heart.
Endocarditis
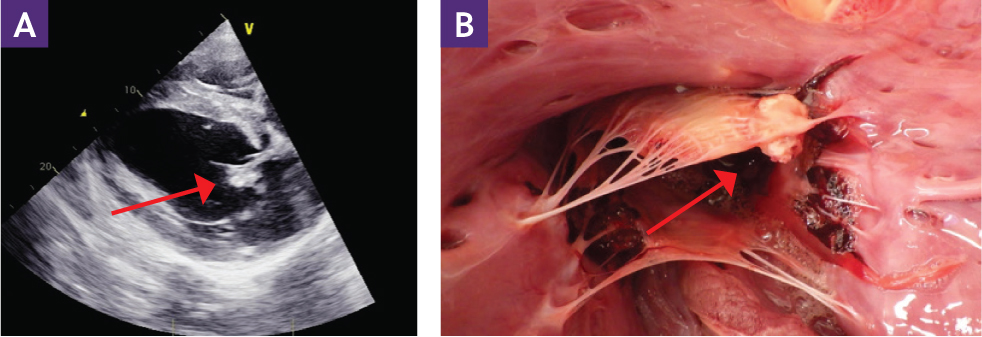
Foals are at increased risk of infective endocarditis, commonly associated with sepsis affecting multiple organs. Pyrexia and a heart murmur are often present but not always, and echocardiography is required for diagnosis (Figure 6) (Marr, 2015).
Myocarditis
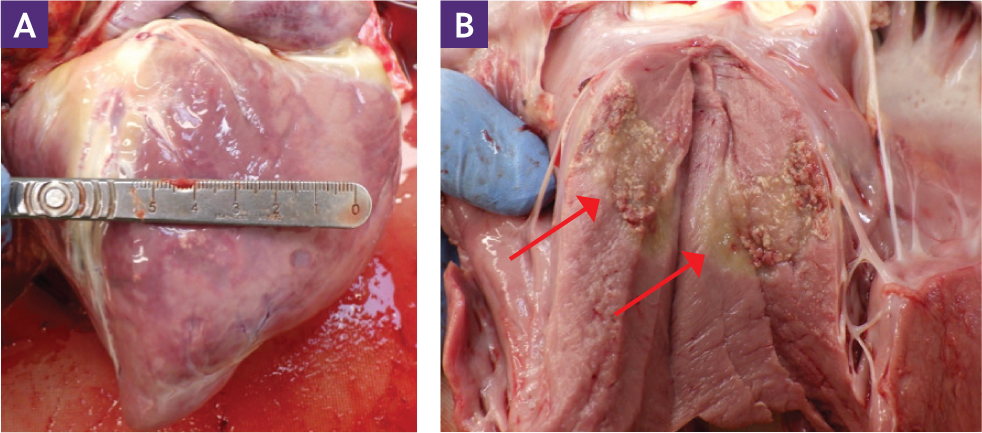
Myocardial disease in foals is rare but can be seen with sepsis (Figure 7) or pathologies such as nutritional myodegeneration (Conze et al, 2022). One study showed significantly higher cardiac tropin-in T and cardiac isoenzyme of creatine kinase in septic foals, but these had no effects on survival (Slack et al, 2005). Blood pressure, echocardiographic and cardiac output measurements help to monitor myocardial function and response to treatment (Marr, 2015). The use of a Holter electrocardiogram is warranted to detect and treat potential associated arrhythmias. Myocardial injury or infarction associated with cardiopulmonary cerebral resuscitation in neonates could have longer-term effects, such as myocardial fibrosis, at an older age (Ruby et al, 2018).
Pericarditis
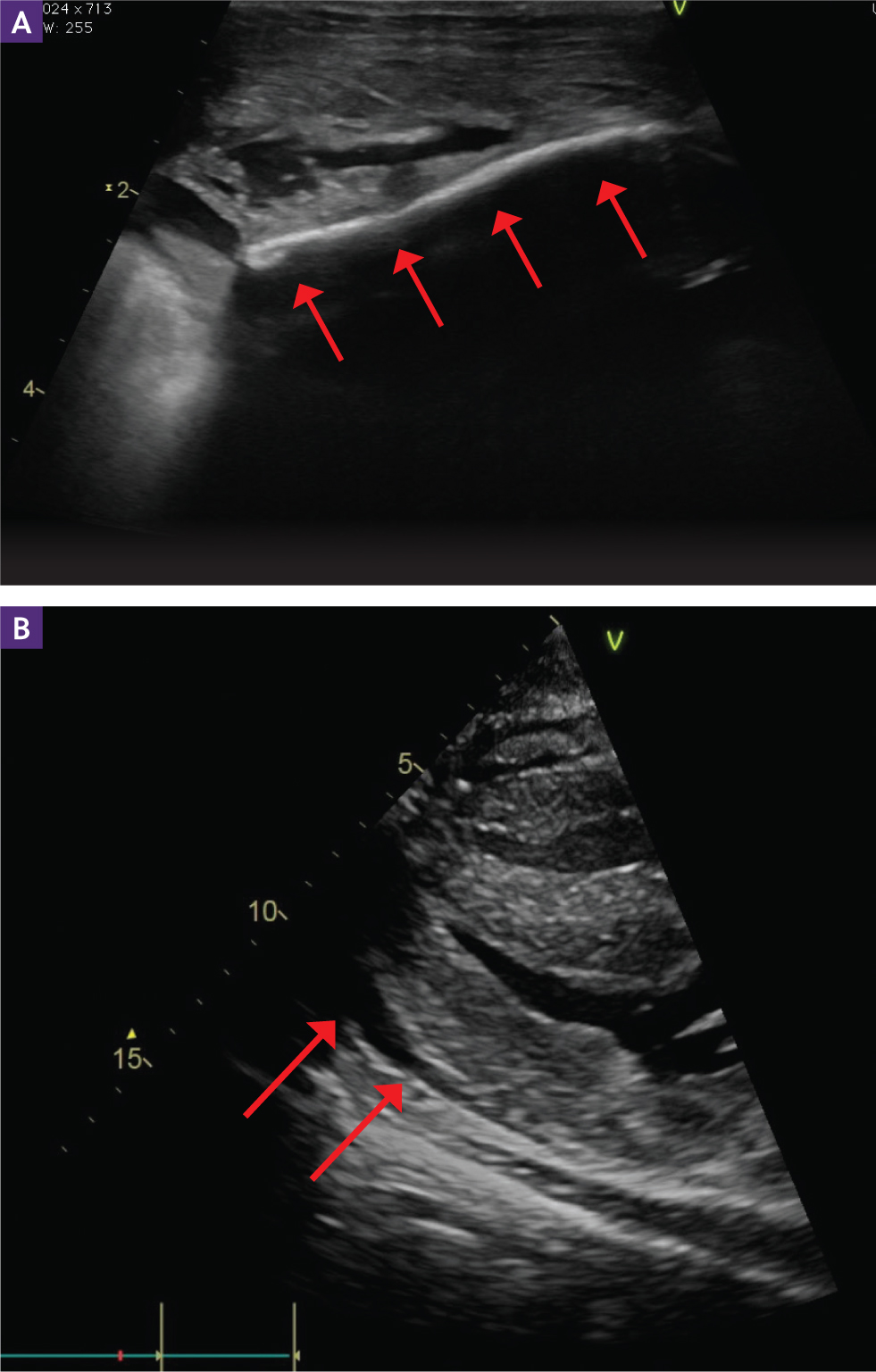
Pericarditis is a rare condition associated with sepsis or systemic inflammatory response syndrome in foals, and only a few cases have been reported (Armstrong et al, 2014). Cardiac auscultation can reveal muffled heart sounds, and the foals are often tachycardic, tachypnoeic and pyrexic (Armstrong et al, 2014). Echocardiography shows fluid and, in some cases, fibrinous material in the pericardial sac, and atrial and ventricular filling are reduced (diastolic heart failure). Thoracic radiography reveals cardiomegaly and possible associated pleural effusion (Armstrong et al, 2014; Marr, 2015). Treatment for pericarditis consists of antimicrobials and pericardial drainage, but the rare cases reported in foals did not survive (Armstrong et al, 2014).
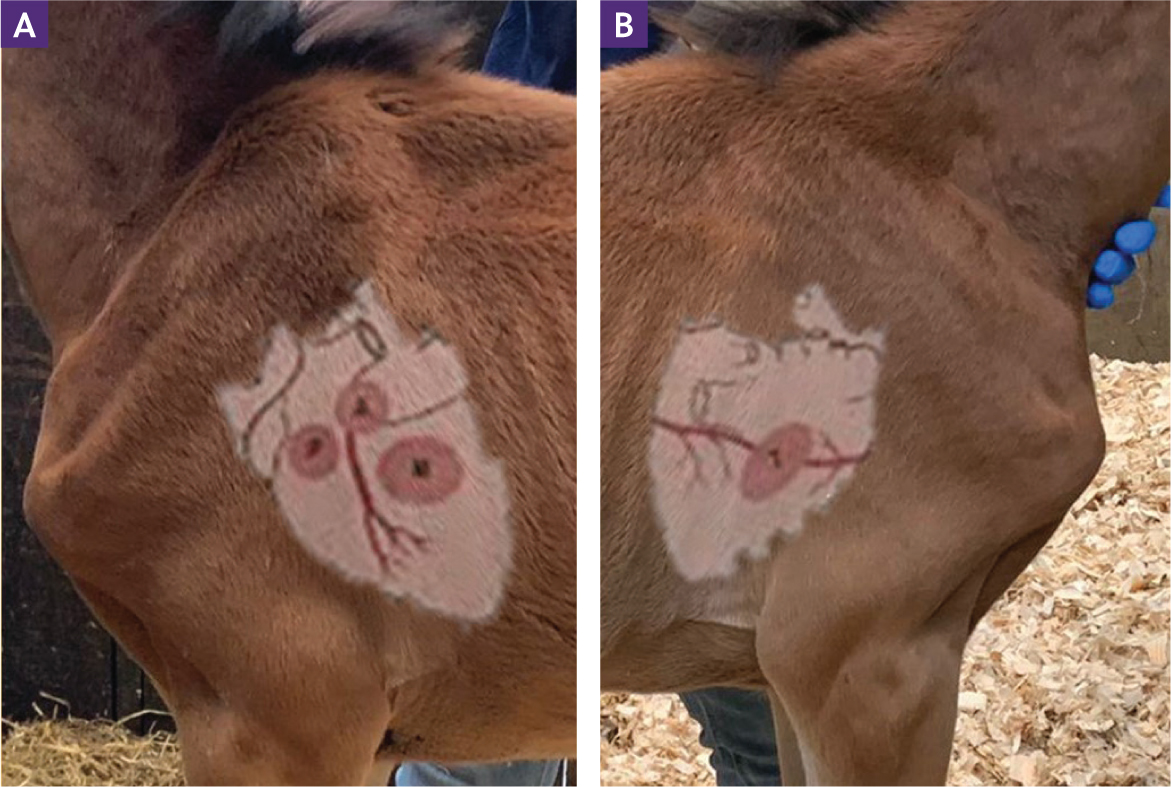
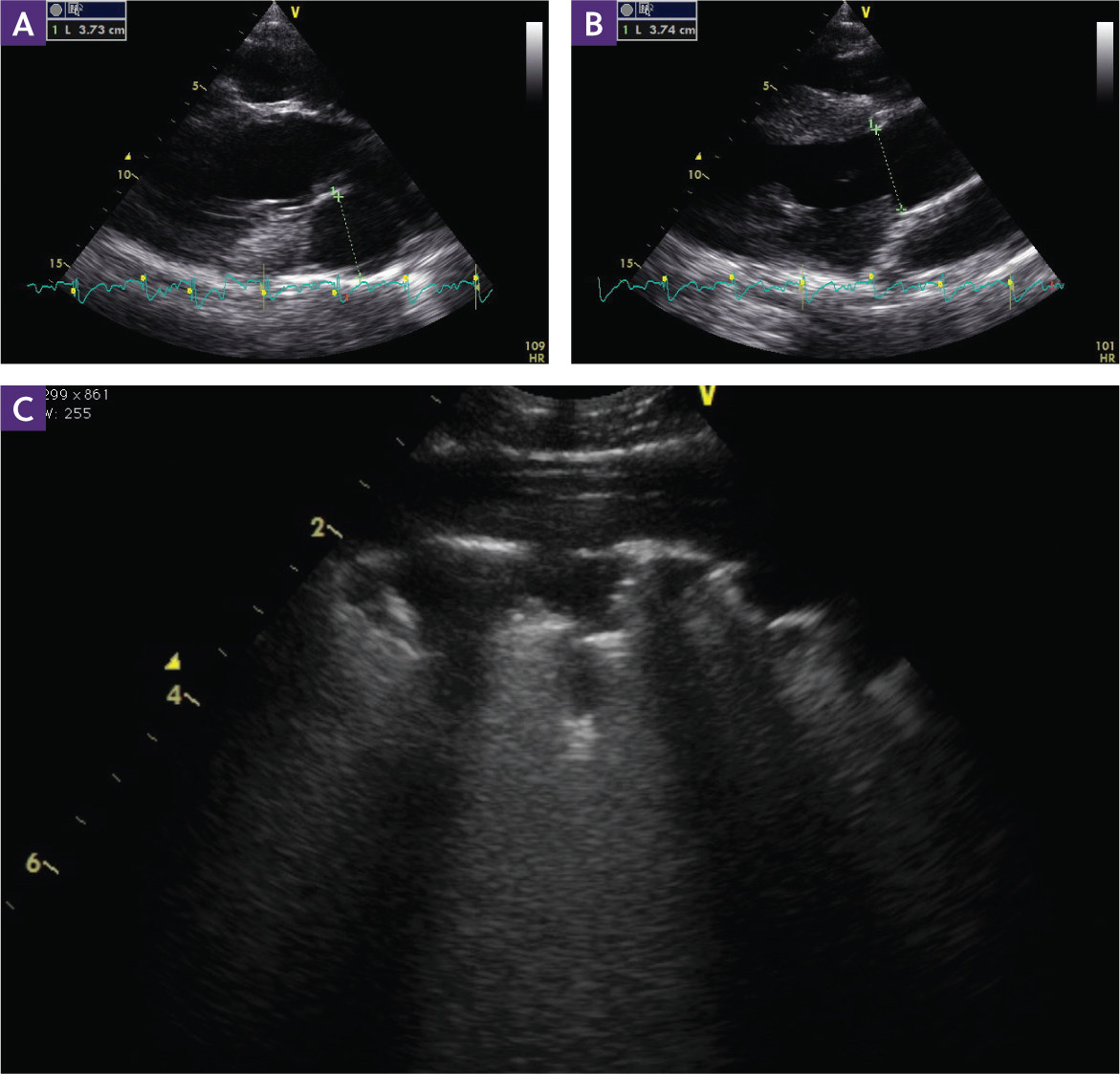
Trauma
Trauma to the heart is a potential consequence of rib fractures and can also be iatrogenic (Marr, 2015). Healthy foals with rib fractures often remain relatively asymptomatic, and conservative treatment with analgesics and restricted exercise is sufficient. However, foals that are recumbent are more prone to intrathoracic complications when multiple or displaced fractures occur; there is a risk for haemothorax, lung contusion, pericardial, myocardial, diaphragmatic trauma and herniation. Diagnosis of rib fractures in foals is made by careful palpation of the thorax, and careful ultrasonography (Figure 8) is more reliable than thoracic radiography. Computed tomography can be performed in complex cases for surgical planning (Jean et al, 2007; Marr, 2015).
Pulmonary hypertension
Hypoxaemia, sepsis, acidosis and severe respiratory disease can result in pulmonary hypertension in neonates (Figure 9). Pulmonary hypertension can lead to reverse flow through the ductus arteriosus and foramen ovale, which have not yet closed permanently, resulting in reversion to fetal circulation with right-to-left shunting. The latter, also called persistent pulmonary hypertension of the newborn or persistent fetal circulation, will further exacerbate hypoxaemia and create a vicious circle (Bernard and Barr, 2012). Aside from addressing the underlying cause, treatment consists of providing intranasal oxygen, correction of acid-base imbalances and eventually administration of pulmonary vasodilators, such as endothelin-1 receptor antagonists and phosphodiesterase inhibitors (Magdesian, 2014).
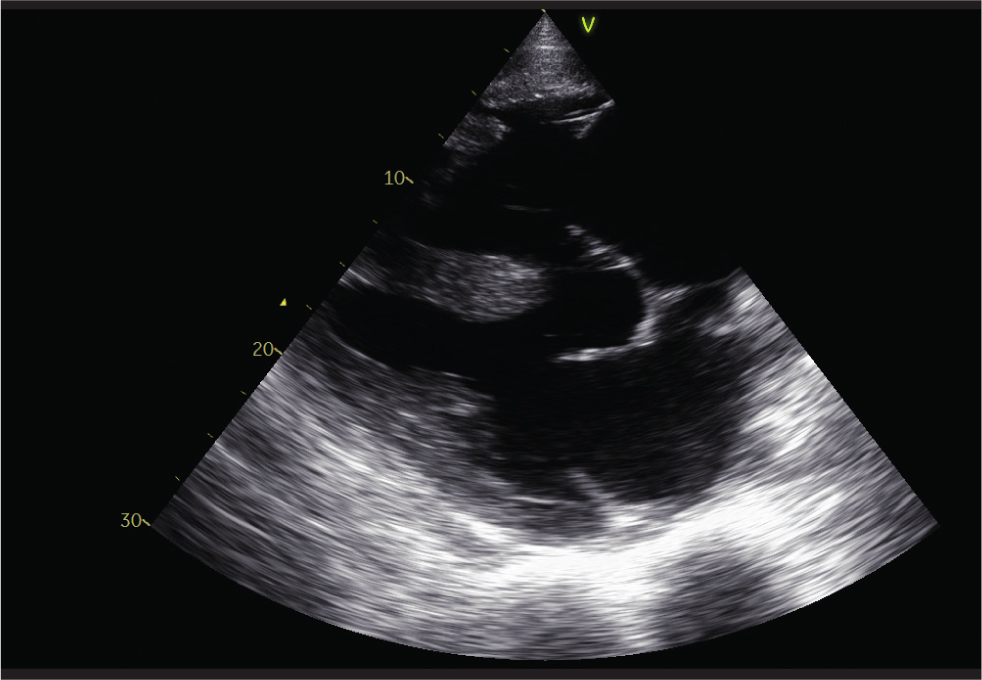
Congenital cardiac anomalies
Congenital cardiac disease is fairly uncommon in horses – the Arabian breed is the most affected (Buergelt, 2003; Schmitz et al, 2008; Hall et al, 2010; Krüger et al, 2016). Many foals with congenital disease may cope well during the neonatal period and, depending on the severity of the disease, only show symptoms at older ages (Marr, 2015). No hereditary studies have addressed congenital cardiac anomalies, but a genetic component has been shown for atrial fibrillation in Standardbreds, and a familial risk for ventricular septal defects in Welsh Mountain ponies and Standardbreds is suspected (Physick-Sheard et al, 2014; Scansen, 2019). In horses, ventricular septal defects are the most common congenital cardiac disease (Figure 10), followed by atrial septum defects, tricuspid atresia and persistent ductus arteriosus. Complex congenital anomalies are rarer; tetralogy of Fallot is the most frequently reported (Figure 11) (Schmitz et al, 2008; Hall et al, 2010; Marr, 2015).
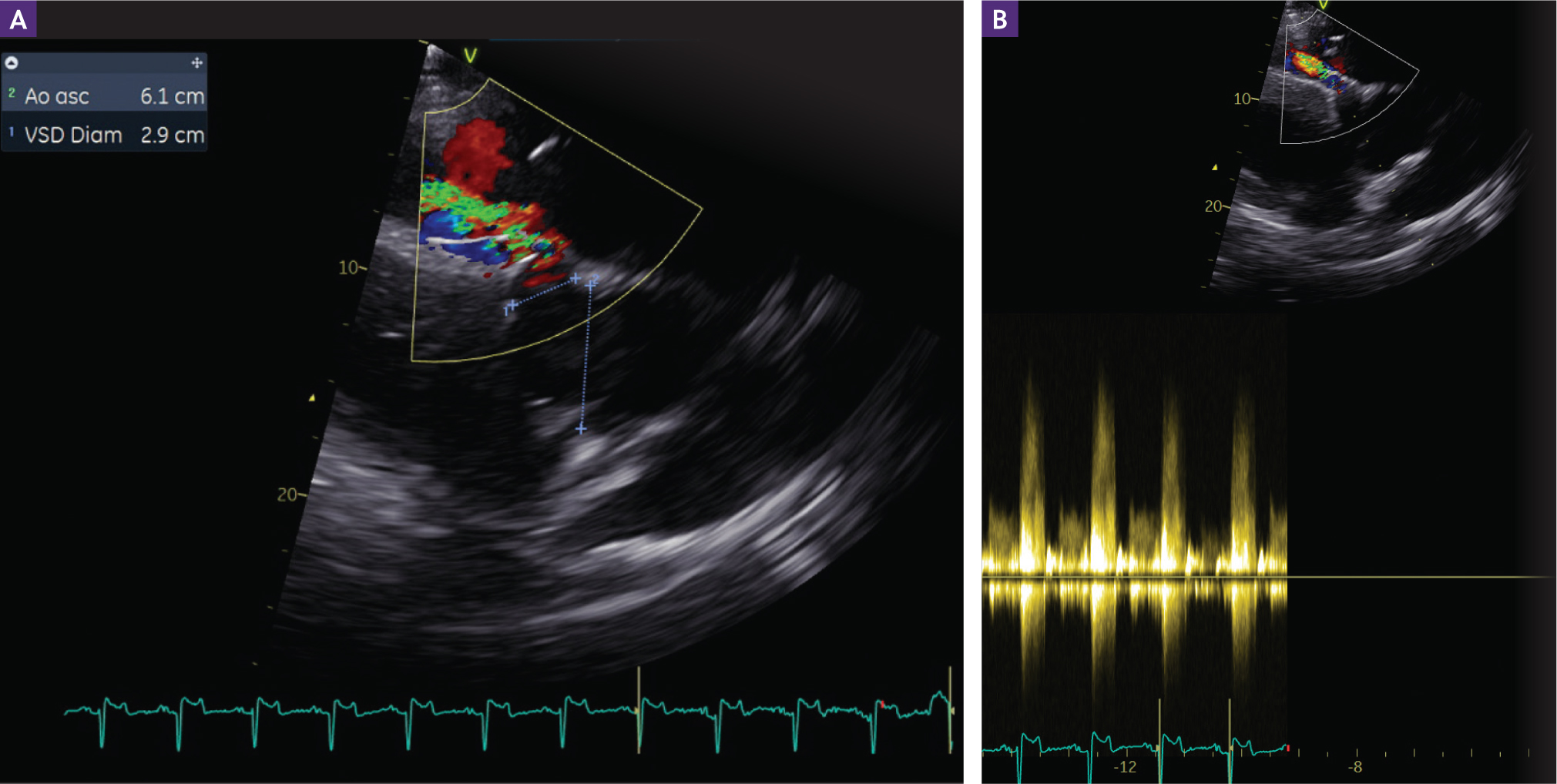
Most congenital heart disease can be divided into three categories: shunts, valvular dysplasia and vascular malformations (Table 4). Shunts are abnormal communications mixing blood between the left and right sides of the circulation. A left-to-right shunt means that blood moves from the systemic circulation towards the pulmonary circulation, and a right-to-left shunt means the deoxygenated blood from the venous systemic circulation is diverted towards the systemic arterial circulation, causing cyanosis (Scansen, 2019).
Conclusions
This article provides a practical overview of the differences between the neonatal and adult cardiovascular system and the most common pathologies associated with the foal's heart. Neonatal foals may experience a number of pathologies, and it is important to bear in mind the difference between adult and neonatal cardiovascular systems when approaching these patients.


